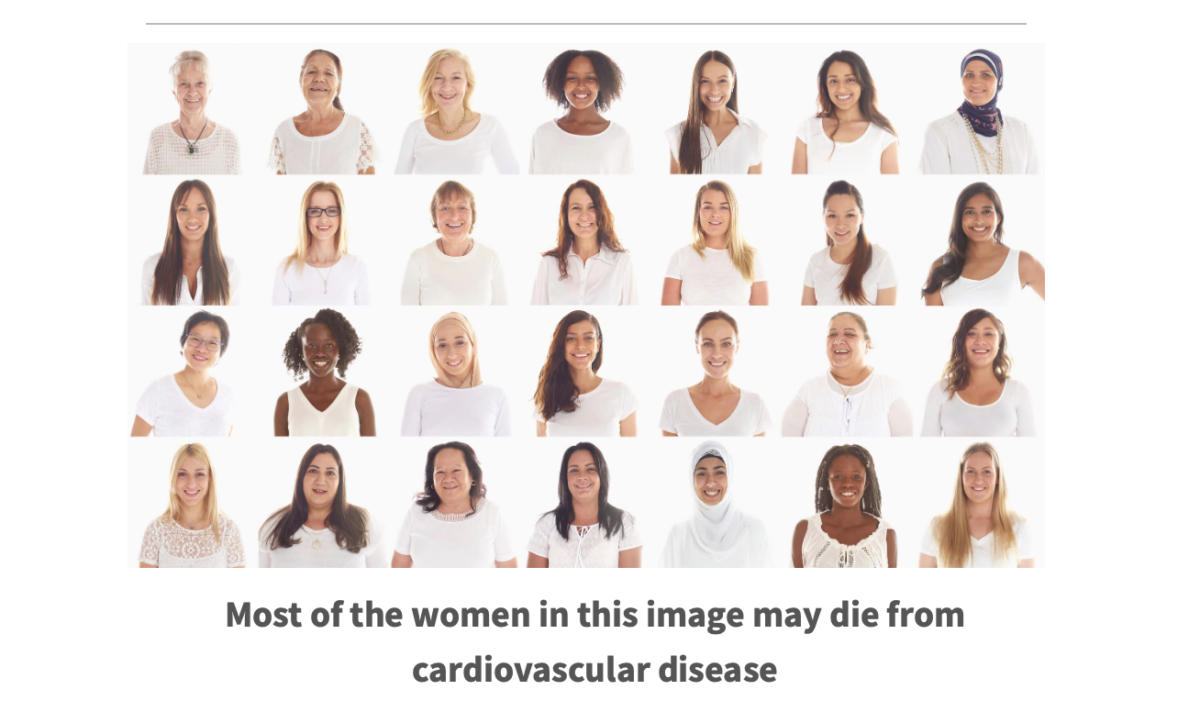
Although the overall mortality due to cardiovascular disease (CVD) is decreasing for both women and men, it is still the leading cause of death for all American women regardless of ethnicity In 2014, females represented nearly half of deaths attributable to CVD. Over the next month, we will provide information on the differences in cardiovascular disease in women compared to men with an emphasis on risk, outcomes, conditions, and treatment.
What is Heart Disease?
Heart disease is a general term that encompasses a range of conditions that affect the heart’s function and structure, an example is heart failure. Cardiovascular disease (CVD) is an even broader term than heart disease which encompasses heart disease and the vessels in the body.
According to the National Heart, Lung, and blood Institute, Coronary heart disease (CHD) encompasses coronary artery disease, coronary microvascular disease, coronary syndrome X, ischemic heart disease, nonobstructive coronary artery disease, and obstructive coronary artery disease. CHD includes acute coronary syndrome (ACS) which is a culprit in ST-elevation myocardial infarction (STEMI), non-ST elevation myocardial infarction (NSTEMI), and unstable angina. CHD is often caused by atherosclerosis, which is also called hardening of the arteries.
Difference in Risk
To understand heart disease in women, it is helpful to start with the risk factors for the condition. Some of the more common risk factors for CHD affect women differently than men. Having several risk factors multiplies the chance of developing CHD. The amplification of these combined risk factors makes it critical to modify those that can be controlled. Risk factors are categorized into non-modifiable and modifiable with prevention efforts targeting the improvement of modifiable risk factors.
Non-Modifiable Risk Factors Can’t Be Changed
- Heredity Risk of developing CVD exists if a parent or sibling had a heart attack at an early age.
- Sex and Age Both sexes have more heart-related problems associated with aging, but women remain at lower risk for the disease than do men at all ages.
- Hormone Changes Menopause significantly changes a women’s estrogen and progesterone levels and is a major consideration when determining a woman’s CVD risk. After menopause when estrogen levels drop, a woman’s likelihood of developing hypertension and subsequent CVD increases and approaches the levels found in men.
Modifiable Risk Factors Can Be Changed
- Smoking While smoking is the biggest preventable risk factor for CHD in both sexes, it is more strongly associated with increased risk in women. Stopping smoking provides an immediate benefit and longer-term decreased risk of heart disease. Nonsmokers are not necessarily safe either. There is a 25% to 30% increased risk of developing CHD for nonsmokers exposed to secondhand smoke.
- Hypertension Not only is hypertension one of the major risk factors for CAD, it also is the biggest for stroke and a major cause of heart and renal failure. When hypertension exists with other risk factors, such as smoking or diabetes, the risk of heart attack greatly increases.
- Hyperlipidemia In general, the higher the low-density lipoprotein (LDL), the greater the risk of CHD. Ideally, optimal lipid levels are achieved and/or maintained through lifestyle approaches such as diet and physical activity. When lifestyle modification does not improve a woman’s lipid profile, the provider may order statins to successfully bring a woman’s lipid profile to a lower risk category.
- Diabetes adversely affects every organ and tissue in the body, including the cardiovascular system. The chronic systemic inflammation caused by frequent hyperglycemia irritates blood vessel walls and contributes to atherosclerosis. In fact, diabetes is so damaging to the heart that compared to women without diabetes, women with diabetes are at more than six times higher risk of death due to CVD.
- Obesity is a major risk factor for CHD and women. Obesity increases CHD risk via several mechanisms. It increases cardiac preload, increases cardiac output, and expands plasma volume. There is an increase in stroke volume and left ventricular filling pressures as demands on cardiac output rise. The link between obesity and CHD is well established. Weight loss can reduce or eliminate hypertension.
- Metabolic Syndrome National Health and Nutrition Examination Survey data from 2011 to 2012 showed that 36.6% of women in the U.S. have metabolic syndrome. Metabolic syndrome is a group of five risk factors:
- Waist measurement greater than or equal to 35 inches (40 inches in men)
- Triglycerides at or above 150 mg/dL or receiving treatment for elevated triglycerides
- HDL less than 50 mg/dL or receiving treatment for low HDL
- Blood pressure at or above 130/85 mmHg (either number) or receiving blood pressure treatment
- Fasting blood glucose at or above 100 mg/dL or receiving treatment for elevated glucose
- When considered individually these risk factors may seem insignificant, but when occurring in a group they greatly increase the risk for CHD. If three out of factors are present, a woman is considered to have metabolic syndrome.
When considered individually these risk factors may seem insignificant, but when occurring in a group they greatly increase the risk for CHD. If three of the factors are present, a woman is considered to have metabolic syndrome.
What You Can Do to Help Your Heart
-
The good news is you can reduce your modifiable risk factors by taking action. If you smoke, quit! Increase your physical activity if you are able to and start making healthier choices about your diet. And reduce your stress. Start with small changes and as you feel better and see results, make additional changes to improve your health.
Your heart will thank you!