Obstructive sleep apnea, when left untreated, can cause serious health problems. These can include excessive daytime sleepiness, high blood pressure, heart failure, cognitive issues, accidents related to sleep loss, depression, poor daytime function, and more. Yet, about 80 to 90 percent of people with obstructive sleep apnea haven’t been diagnosed.
If you have obstructive sleep apnea, you might experience symptoms like difficulty staying asleep, loud snoring, morning headaches, and waking up feeling unrefreshed. This is mostly because the condition interrupts breathing during sleep, leading to non-restorative rest.
Let’s take an in-depth look at obstructive sleep apnea, from causes and symptoms to diagnosis and treatment.
What is Obstructive Sleep Apnea?
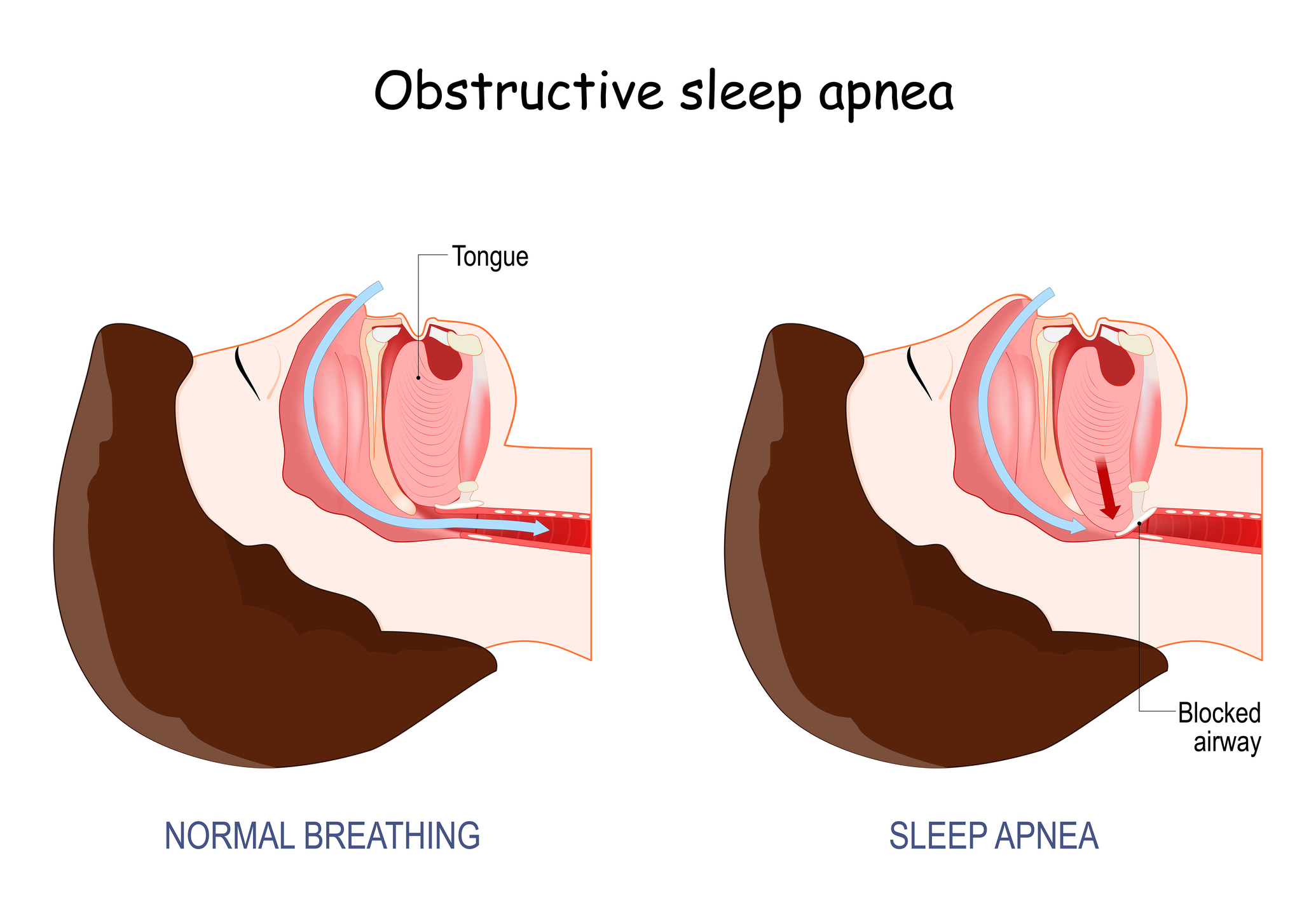
Obstructive sleep apnea is a sleep-related breathing disorder. It causes the upper airway to partially or completely collapse, reducing or stopping airflow. This can occur even when you try to breathe while asleep, and can last for at least 10 seconds.
OSA causes interruptions in normal breathing that last for 10 seconds to a minute, or more. You might choke or gasp as you begin breathing naturally again. A person can have hundreds of these episodes each night, leading to disturbed and unrefreshing sleep.
Although OSA can cause loud snoring, most people who snore don’t have OSA. Also, this condition runs in families, with 25 to 40 percent of cases having a family history.
OSA is grouped according to how severe a person’s symptoms are:
- Mild OSA: Normal breathing is cut off 5 to 15 times an hour
- Moderate OSA: Episodes of interrupted breathing occur 15 to 30 times
- Severe OSA: A person experiences more than 30 episodes of interrupted breathing in an hour. Severe OSA is tied to an increased risk of death in middle-aged men.
How Common is Obstructive Sleep Apnea?
OSA is the most common sleep-related breathing disorder, occurring in one billion people globally. But about 80 to 90 percent of adults with OSA symptoms haven’t been diagnosed. OSA affects two percent of children and is most common in preschool children.
This condition is about four times more common in men and seven times more common in people with obesity. Although anyone can have OSA, this condition affects more people as they grow older.
What are the Symptoms of OSA?
About 85 percent of people with OSA snore loudly. Still, most people that snore don’t have OSA.
If you have OSA, you might also have symptoms like:
- Choking, gasping, or snorting while asleep
- Having restless and fragmented sleep
- Morning headache
- Excessive daytime sleepiness
- Forgetfulness
- Mood changes
- Low sex drive
- Difficulty concentrating
- High blood pressure
- Tiredness
- Waking up with a sore throat or dry mouth.
You might not know you have any nighttime symptoms. If you share a bed with someone or have roommates, they might tell you about them.
Also, even though you might have breathing problems at night, you might not show some daytime signs of OSA. About 24 percent of men and nine percent of women experience nighttime symptoms of OSA but don’t feel sleepy during the day.
What Causes Obstructive Sleep Apnea?
The muscles become more relaxed during sleep. But with OSA, the muscles in the back of the throat relax so much that they drop and partially or completely block the upper airway, disrupting normal breathing for at least 30 seconds.
When your brain notices that you’re not breathing properly, it wakes you up so you can start breathing normally. You might react by choking or gasping as you return to breathing properly.
What are the OSA Risk Factors?
Obesity, older age, and being male are the most common factors that increase the likelihood of a person developing OSA.
Other risk factors for OSA include:
- Alcohol or sedative use
- Having a family history of OSA
- Having a large neck size
- Having a craniofacial abnormality
- Smoking
- Pregnancy
Having underlying conditions may also cause a person to develop OSA. Health problems linked with an increased risk of OSA include:
- Down syndrome
- Endocrine disorders like hypothyroidism and diabetes
- A genetic disorder called Prader-Willi syndrome
- Nervous system disorders like stroke, Parkinson’s disease, and spinal cord injury
- Abnormal heart rhythm
- Heart failure
What are the Complications of Obstructive Sleep Apnea?
OSA is a serious medical condition; when a person doesn’t treat it, they become prone to developing other health problems like:
- High blood pressure
- Abnormal heart rhythm
- Excessive sleepiness
- Depression
- Nonalcoholic fatty liver disease
People with untreated OSA may also be at risk of experiencing sleep loss-related accidents like car accidents. Excessive sleepiness may also result in poor job performance or job loss and poor sex life.
People who share the same space with people with OSA may also experience poor sleep quality from disturbances from their partner’s nighttime symptoms.
OSA may also increase your risk of complications like cardiac arrest after surgery. Talk to your doctor if you have OSA symptoms before undergoing surgery. Your doctor may put you on continuous positive airway pressure (CPAP) treatment when you’re on preoperative medications and recovering.
Studies suggest that people with OSA are at eight times the risk for COVID-19 and are more likely to be hospitalized or develop respiratory failure due to COVID-19 infection.
When Should You See a Doctor?
You should see a doctor if you or your bed partner notices symptoms like:
- Loud, disruptive snoring
- Waking up to holding your breath, gasping, or choking
- Dozing off or feeling sleepy all-day
- Breath pauses while asleep
- Tiredness
- Irritability
- Waking up tired
How is Obstructive Sleep Apnea Diagnosed?
Before your doctor diagnoses you with OSA, they’ll look at your daytime and nighttime symptoms and monitor your sleep to check if you have
- at least five episodes of interrupted breathing an hour with other nighttime symptoms like loud snoring
- or at least 15 episodes of breath pauses without symptoms.
They’ll look at least one of the following signs of OSA:
- Nighttime symptoms like waking up gasping, choking, or snorting
- Daytime symptoms like daytime sleepiness, dozing off during the day, tiredness, waking up feeling unrefreshed, and interrupted sleep.
- Bed partner report that you snore loudly or have breathing interruptions.
Your doctor may ask about how you’ve been sleeping, look through your medical history, and do a physical exam checking your nose, mouth, neck, or throat for abnormalities that may make you prone to having OSA, like a nasal obstruction. You might also get tested for conditions linked with OSA, like hypothyroidism.
When necessary, your doctor may refer you to a sleep specialist for further testing, who will then diagnose you, identify how severe your symptoms are, and prescribe treatment accordingly.
Here are tests you may undergo for an OSA diagnosis:
Polysomnography
Polysomnography, a sleep study, is a gold standard test for diagnosing OSA and other sleep-related breathing disorders and the best way to confirm that a person has OSA.
You will take this sleep study at a sleep lab or sleep center, where you’ll be monitored all night. This procedure uses equipment to record your breathing patterns, brain activity, eye movement, muscle activity, heart rate and rhythm, blood oxygen level, and body position while you’re asleep.
A sleep specialist may use polysomnography to check for other sleep disorders. After this test, the sleep specialist will identify how many episodes of disturbed breathing you had and how severe your symptoms are.
Home sleep testing
You can also do an at-home sleep test with portable devices that test for OSA and its severity. These devices record heart rate, blood oxygen levels, breathing effort, and airflow.
You’ll take this test with the guidance of an experienced sleep technologist or technician following American Academy of Sleep Medicine (AASM) guidelines.
How is Obstructive Sleep Apnea Treated?
OSA treatment is long-term and focuses on treating signs and symptoms of OSA, improving sleep quality, and regulating breathing at night and blood oxygen levels.
Your treatment might include:
Weight management
A doctor may recommend weight management and exercise for people with obesity or people who are overweight.
A weight management program might include a nutrition or diet plan, following an exercise routine, drug therapy, or making lifestyle changes.
Although having a healthy weight may not cause your symptoms to go away completely, you might notice improvements in your symptoms, how you sleep, and daytime functioning.
Avoiding alcohol
If you take alcohol, your doctor may advise you to quit. It can worsen OSA symptoms, cause weight gain, and lower sleep quality.
Alcohol can also trigger OSA episodes in people who snore but don’t have OSA.
Avoiding certain medications
Some medications, including those that work on the central nervous system, can worsen a person’s OSA symptoms.
Medications your doctor might avoid prescribing to you when you have OSA include:
- Anti-anxiety medications
- Sleeping pills
- Antiepileptic drugs
- Sedating antidepressants
- Antihistamines
Positive airway pressure (PAP) therapy
Positive airway pressure (PAP) therapy involves using a device to deliver a stream of air under pressure into the airway to keep it open during sleep so a person can breathe normally throughout the night.
Continuous positive airway pressure (CPAP), a type of positive airway pressure therapy, is the go-to, simplest, and most effective treatment for people with moderate to severe OSA.
A doctor might also recommend bilevel positive airway pressure (BPAP) or auto-titrating positive airway pressure (APAP) when necessary to treat OSA.
Changing your sleeping position
Positional obstructive sleep apnea is OSA that happens twice more frequently when you sleep on your back than in any other position. More than 50 percent of people with OSA have positional obstructive sleep apnea.
Sleeping on your back can worsen OSA symptoms. Gravity makes it more likely that your airway can be obstructed when you sleep on your back, making you prone to having more OSA episodes.
Most people with OSA say that their OSA symptoms improve when they sleep on the couch. This improvement might happen because most people are less likely to lie on their back when on the couch.
If you sleep on your back, consider changing your sleep position to your stomach or side to reduce OSA and improve your symptoms.
You can also get positional therapy devices that train you to sleep in other positions aside from your back may help change your sleeping position from back to side or stomach sleeping.
This treatment may be beneficial for people with mild to moderate OSA.
Oral appliances
A doctor might recommend oral appliances for people who can’t use CPAP or have mild to moderate OSA.
Some oral devices push the lower jaw forward, so there are no airway blockages. Others pull the tongue, so it doesn’t obstruct the airway. Your doctor may tell you the right oral appliance for you.
Surgery
Your doctor might recommend surgery when positive airway pressure therapy or oral appliances don’t improve your symptoms. It will also be the first treatment choice when anatomic features block the upper airway.
Surgery for OSA is grouped into:
- Nasal procedure
- Lower pharyngeal procedure
- Upper pharyngeal procedure
- Upper airway surgery
The goal of any surgical procedure is to expand or keep the upper airway steady. Your doctor will choose surgery depending on:
- How severe your symptoms are
- Your anatomy
- Any risk factors
- What you prefer
Obstructive sleep apnea is a sleep-related breathing disorder that can significantly alter a person’s sleep health and daytime functioning and increase the risk of other health problems. If you or someone else notices symptoms of this disorder, it’s best to see a doctor immediately. They can diagnose you and recommend necessary treatment.
Resources
- Obstructive Sleep Apnea: https://www.msdmanuals.com/professional/pulmonary-disorders/sleep-apnea/obstructive-sleep-apnea
- Obstructive Sleep Apnea: https://aasm.org/resources/factsheets/sleepapnea.pdf
- Obstructive Sleep Apnea: https://www.ncbi.nlm.nih.gov/books/NBK459252/
- Obstructive sleep apnea: https://www.mayoclinic.org/diseases-conditions/obstructive-sleep-apnea/symptoms-causes/syc-20352090
- Polysomnography: https://pubmed.ncbi.nlm.nih.gov/31277862/
- Polysomnography: https://www.mayoclinic.org/tests-procedures/polysomnography/about/pac-20394877#:
- Management of obstructive sleep apnea in adults: https://www.uptodate.com/contents/management-of-obstructive-sleep-apnea-in-adults
- Positive Airway Pressure (PAP) Therapies: https://stanfordhealthcare.org/medical-treatments/p/positive-airway-pressure-therapies.html
- Surgical treatment of obstructive sleep apnea in adults: https://www.uptodate.com/contents/surgical-treatment-of-obstructive-sleep-apnea-in-adults
- Usage of Positional Therapy in Adults with Obstructive Sleep Apnea: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4298770/#B8
-
- Positional Obstructive Sleep Apnea: https://www.sleepassociation.org/sleep-apnea/positional-sleep-apnea/
- Positional Therapy Is Worth a Try in Patients with Mild Obstructive Sleep Apnea: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4298780/
- Positional Sleep Aids Comparison Guide: https://sleepreviewmag.com/sleep-treatments/therapy-devices/positional-therapies-supine/positional-sleep-aids-guide/



