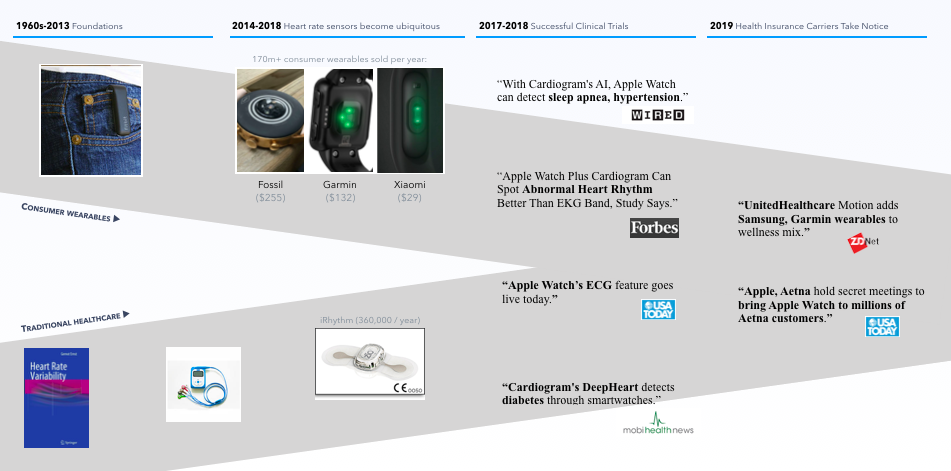
Consumer wearables and traditional healthcare are on a collision course. The 170+ million wearables sold per year dwarf the scale of traditional medical devices, and they come with increasingly powerful health sensors. Multiple studies have now shown accurate detection of several health conditions using consumer wearables like Apple Watch, Garmin, and WearOS by Google paired with AI-based algorithms:
- Atrial fibrillation: the mRhythm Study (Heart Rhythm Society), Apple Heart Study (American College of Caridology)
- Hypertension: Cardiovascular Risk Stratification Using Off-the-Shelf Wearables and a Multi-Task Deep Learning Algorithm (American Heart Association Scientific Sessions)
- Sleep apnea: same AHA study as above.
- Diabetes: DeepHeart: Semi-Supervised Sequence Learning for Cardiovascular Risk Prediction (AAAI-2018).
But if we can detect a health condition, should we? The answer partly depends on which health condition.
What follows is a summary of the evidence and guidelines around each of these four health conditions.
Atrial Fibrillation
Atrial fibrillation is the most common abnormal heart rhythm, but screening for it is particularly controversial because its main treatment—anti-coagulants—prevents ischemic strokes but causes brain hemorrhage. The benefits and harms are both significant. One cardiologist described anti-coagulation to me as navigating between Scylla and Charybdis— too little anti-coagulation, and you’ll fail to prevent an ischemic stroke; too much, and you’ll cause a hemorrhagic stroke. As a result, the decision to screen is not a clear “no-brainer.”
For that reason, the US Preventive Services Task Force (USPSTF) gave an “I” rating (insufficient evidence to judge the benefits vs harms) to AF screening. When a patient visits a doctor with atrial fibrillation detected from their watch, physicians will likely use their CHA₂DS₂-VASc score to navigate between Scylla and Charybdis. CHA₂DS₂-VASc predicts the the risk of stroke based on factors like presence of high blood pressure, diabetes, heart failure, and so on, although it’s not hard to imagine a near future where simple rules like CHA₂DS₂-VAS are replaced by more sophisticated, AI-based models.
High Blood Pressure
30% of people have high blood pressure, and research presented by Cardiogram and UCSF Cardiology at the American Heart Association’s Scientific Sessions showed 82% accuracy at detecting people with high blood pressure using DeepHeart.
So if we can detect people with undiagnosed high blood pressure, should we? The answer is generally yes — the US Preventive Service Task force rates screening for high blood pressure in adults as an “A”. There’s a clear, cost-effective mechanism to confirm a diagnosis (ambulatory or at-home blood pressure monitoring), the benefits are clear (reduced stroke, heart failure, and heart attacks), and there are few major harms of blood pressure medication or lifestyle changes.
As a result, by law, health insurers actually must provide first-dollar coverage for hypertension screening — it’s not subject to your deductible, co-insurance, or co-pays.
Sleep Apnea
About 80% of people with sleep apnea are undiagnosed. Our research shows roughly 90% accuracy in detecting sleep apnea using consumer wearables, and confirmation can be done via accurate, cost-effective, at-home sleep tests.
So should we screen for sleep apnea? The most common treatment is CPAP, and USPSTF identified evidence of clinical benefits (reductions in blood pressure, AHI, and ESS score) and evidence that the harms (oral or nasal dryness, rash, etc.) are small. Since simply giving every adult in the US an at-home sleep test would be prohibitively expensive (roughly $60B), the “critical gap” identified by the USPSTF was an accurate, cost-effective way to detect people at elevated risk of sleep apnea (which is typically done using self-reported surveys). As a result, the USPSTF rating is currently an I.
Fortunately, pre-screening is exactly the gap that wearables can fill. Consumer wearables that people are buying already, paired withan algorithm like DeepHeart, can cheaply and effectively identify those most likely to have sleep apnea, who can then be offered a confirmatory sleep test and guided effective treatments like CPAP. These programs can even be remarkably cost-effective—one study of sleep apnea screening showed cost savings of $2,400 in the first year.
Diabetes
Maybe most remarkably, wearable heart rate sensors have shown the ability to detect signs of diabetes. The link between heart rate and diabetes comes from your autonomic nervous system, which connections your pancreas, blood vessels, and more to your heart—multiple studies, including ARIC, have linked high resting heart rate and low HRV to risk of diabetes. The US Preventive Services task force rates diabetes screening a “B,” and like hypertension, health insurers are required to provide first-dollar coverage by law.
Device-Agnostic Population Health
Last, it’s worth remembering that the consumer wearable market is highly fragmented along platform (iPhone vs Android), form factor (smart watch vs fitness tracker), battery life, price ($29 Xiaomi vs $255 Fossil vs $399 Apple Watch Series 4), and fashion (round, rectangular, size, thickness, finish, etc.).
According to IDC, the top three wearable makers combined make up less than half the market:
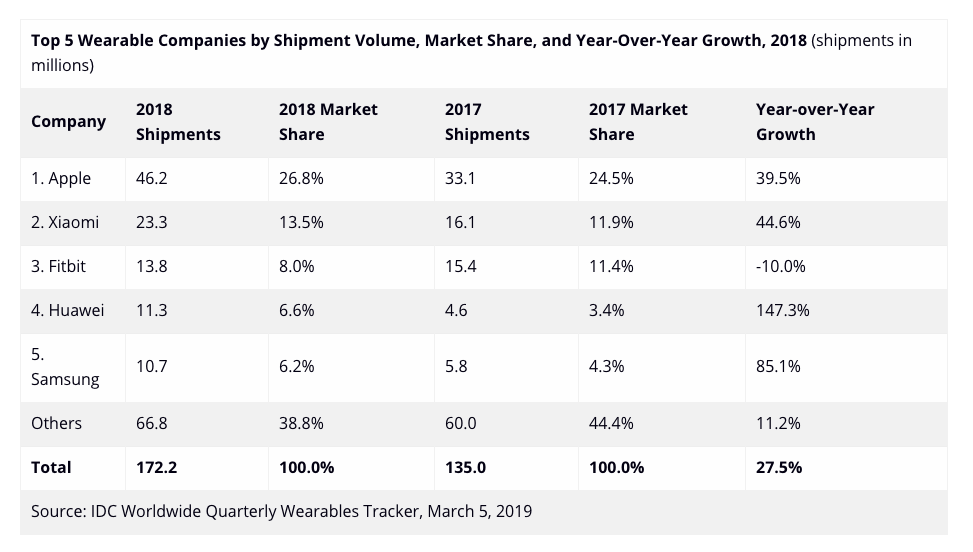
That means the most successful approaches to population health screening will need to be device-agnostic. That’s part of why we launched Cardiogram for Garmin and WearOS by Google, with more platforms coming.
What's Next?
Large parts of medicine will be reinvented in the next few years. If you’re interested in building primary care of the future using the consumer wearables of today—either as an insurer or employer partner, or member of our team—please reach out at [email protected]!