A migraine headache is usually an intense, throbbing pain on one, or sometimes both, sides of the head. Migraine is the most common form of disabling headache that sends patients to see their doctors.
These disabling headaches affect significantly more women than men. In fact, migraine pain and symptoms impact 29.5 million Americans alone, and three out of four people who have migraines are women.
What are common migraine symptoms for women?
Most women with migraines feel the pain in the temples or behind one eye or ear, although any part of the head can be involved. Besides pain, migraine can also cause sensitivity to light and sound as well as nausea and vomiting. Some may also see spots or flashing lights or have a temporary loss of vision.
What are common risk factors in women with migraine?
While we don’t know exactly what causes migraines, we know that being a woman is one of the greatest risk factors. However, there are some other commonalities in those who experience them:
- Those between the ages of 15 and 55 (they becomes less severe and frequent with age)
- Those with high levels of stress
- Those with a family history of migraine or disabling headache
The exact cause of migraine is not fully understood. However, most researchers think they're due to abnormal changes in levels of substances that are naturally produced in the brain. When the levels of these substances increase, they can cause inflammation. This inflammation then causes blood vessels in the brain to swell and press on nearby nerves, causing pain.
What are common migraine triggers for women?

Experts know that people with migraines react to a variety of factors and events, called triggers. These triggers can vary from person to person and don't always lead to migraine.
It’s not overly shocking that a combination of triggers — not a single thing or event — is more likely to set off an attack. A person's response to triggers can also vary from migraine to migraine.
Many women with migraine tend to have attacks triggered by any combination of the following events:
- Lack of or too much sleep
- Skipped meals
- Bright lights, loud noises, or strong odors
- Hormone changes during the menstrual cycle
- Stress and anxiety, or relaxation after stress
- Weather changes
- Alcohol (often red wine)
- Caffeine (too much or withdrawal)
- Foods that contain nitrates, such as hot dogs and lunch meats
- Foods that contain MSG (monosodium glutamate), a flavor enhancer found in fast foods, broths, seasonings, and spices
- Foods that contain tyramine, such as aged cheeses, soy products, fava beans, hard sausages, smoked fish, and Chianti wine
- Aspartame (NutraSweet® and Equal®)
Stress as a Migraine Trigger for Women
Stress can trigger both migraine and tension-type headache. Events like getting married, moving to a new home, or having a baby can often cause stress in women.
Interestingly, studies show that everyday stresses — not major life changes — cause most headaches. For many women, this can look like juggling many roles, such as being a mother and wife, having a career, and taking on financial pressures.
Ways of Dealing with Daily Stressors
Making time for yourself and finding healthy ways to deal with stress is important. Some things you can do to help prevent or reduce stress include:
- Eating healthy foods
- Being active (at least 30 minutes most days of the week is best)
- Doing relaxation exercises
- Getting enough sleep
Other Lifestyle Changes for Reducing Migraine Frequency
One of the other most important things you can do for lowering stress levels is to figure out what it is that causes you to feel stressed in the first place. By becoming aware of your stressors, you may be able to cut some of them out.
For example, if driving to work is stressful, try taking the bus or subway. You can take this time to read or listen to music, rather than deal with traffic. For stressors you can't avoid, staying organized and doing as much as you can ahead of time will help you to feel in control.
Changing your lifestyle to practice healthy habits can also reduce number of migraine attacks:
- Avoid or limit triggers.
- Get up and go to bed the same time every day.
- Eat healthy foods and do not skip meals.
- Engage in regular physical activity.
- Limit alcohol and caffeine intake.
- Learn ways to reduce and cope with stress.
The Role of Hormones in Women's Migraine
It's been shown that one of the main reasons women are more likely to suffer from migraines is due to their fluctuations in hormones. Let's explore this further:
How do periods impact migraines?
More than half of migraines in women occur right before, during, or after a woman has her period. This is often called "menstrual migraine." However, only a small fraction of women who have migraine around their period only experience migraine at this time; Most have migraine headaches at other times throughout the month as well.
How exactly the menstrual cycle and migraines are linked is still unclear. However, we know that just before the cycle begins, levels of the female hormones, estrogen and progesterone, decrease sharply. This drop in hormones may trigger a migraine as estrogen controls chemicals in the brain that affect a woman's pain sensation.
How does menopause impact migraines?
If your migraine headaches are closely linked to your menstrual cycle, menopause may make them less severe. As you get older, symptoms such as nausea and vomiting may decrease as well. In fact, about two-thirds of women with migraines report that their symptoms improve with menopause.
However, this isn't the case for all women. For some, menopause actually worsens migraine or even triggers them to start. It's not clear why this happens. Menopausal hormone therapy, which is prescribed for some women during menopause, may be linked to migraines during this time. In general, though, the worsening of migraine symptoms goes away once the process of menopause is complete.
How does hormonal birth control impact migraines?
In some women, birth control pills improve migraine. The pills may help reduce the frequency and severity of attacks. However, in other women, the pills may worsen their migraines. And still in others, taking birth control pills has no effect on their migraines whatsoever.
The reason for these different responses is not well understood. For women whose migraines get worse when they take birth control pills, their attacks seem to occur during the last week of the cycle. This is because the last seven pills in most monthly pill packs don't contain hormones; they are simply there to keep you in the habit of taking your birth control daily. Without the hormones, your body's estrogen levels drop sharply which may trigger migraine in some women.
Talk with your doctor if you think birth control pills are making your migraines worse. There are options such as switching to a pill pack in which all the pills for the entire month contain hormones or to a different form of birth control.
Using Migraine IQ to Discover & Manage Your Triggers
Your Migraine IQ app has multiple powerful features for better understanding your migraines and gaining greater control of symptom management.
log your headaches
Anytime you have a migraine headache, use the Migraine IQ Log a Headache feature. Log a Headache will keep track of the date and start time of your headache, allow you to select the location and intensity of your headache pain, and allow you to record your stress levels, possible triggers, symptoms, and medications.
Be sure to use the comment function to document the day of your cycle or Create a Tag for the start date of your cycle.
keep a Daily log
To pinpoint your migraine triggers, use your Migraine IQ daily log.
For now, Migraine IQ allows you to capture triggers that are scientifically-validated by published medical literature. In the future, we will add triggers that are common to many of our users.
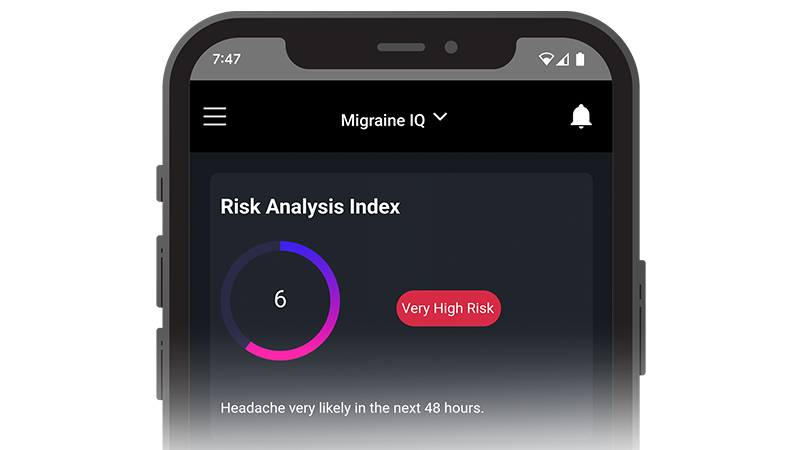
Discover your daily risk index
Your daily Risk Index forecast shares your likelihood of developing a migraine each day.
Based on your daily reports, you can take appropriate action for preventing migraine symptoms and go about your day as you see fit, allowing you to take back control of your life.
Learn more about the Risk Index feature here.
Share data with your doctor
With your Share-with-Doctor feature, you and your doctor can have access to the bigger picture of your migraines. This also allows you both to see if your headaches occur at the same or similar time as your period, or if there are any other common factors related to your migraine episodes.
Your Migraine IQ Share-with-Doctor feature will generate a PDF report that is specific to you, the headaches, triggers and symptoms you have logged using Migraine IQ.
Your individualized report will document specific information that’s valuable to your doctor including:
- Frequency of your migraines
- Location and severity of pain
- How long the headaches last
- When the headaches happen, such as during your period
- Other symptoms, such as light or sound sensitivity and/or nausea and vomiting
- All the medicines that you took to either prevent getting the migraine or to alleviate pain after you had the migraine.
- Reported stress levels, daily activity
Learn how to use your Share-with-Doctore report here.
Enroll in a habit
Because engaging in regular exercise, getting good sleep, and managing stress levels all help improve migraine symptoms, enrolling in one of Cardiogram's healthy habits can help keep you accountable in sticking to them.
If you or a loved one suffer from migraines and headaches, regain control with Migraine IQ and our new Risk Indexfeature. Start by trying our FREE 30-Day Migraine IQ Trial now!



